If you ask any doctor or nurse about what slows their workflow the most, chances are “prior authorization paperwork” will be at the top of the list.
Every day, healthcare providers have to juggle multiple tasks like faxes, phone calls, and forms just to get approval for treatments and prescriptions for their patients.
However, now things are changing. Many healthcare providers are ditching the old manual prior authorization approval process and moving towards electronic prior authorization (ePA).
In this blog, we’ll understand why healthcare providers are making this shift from manual to an electronic authorization system.
What is the Primary Purpose of Prior Authorization in Healthcare?
The main purpose of prior authorization services is to make sure that a certain treatment, procedure, or medication is both medically necessary for the patient and can be covered in the insurance plan. This process helps ensure that the care being provided is appropriate, safe, and inexpensive.
For example, if a patient is prescribed an expensive brand-name medicine, the insurance company may check if there’s a cheaper generic option that works just as well before getting prior authorization for prescription.
In short, prior authorization ensures that healthcare decisions are thoughtful, evidence-based, and focused on the patient’s best outcome.
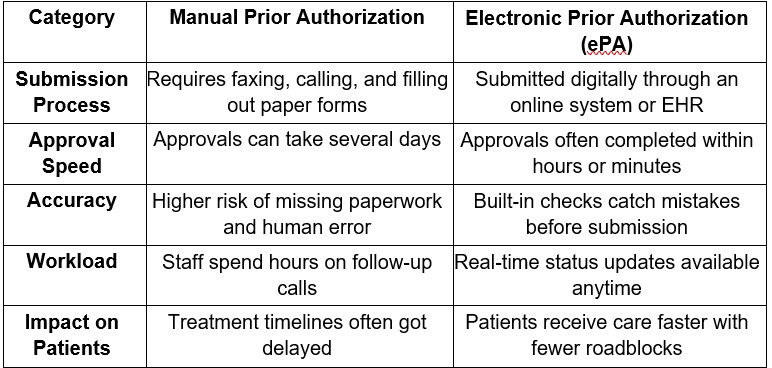
Difference Between Electronic and Manual Prior Authorization
When it comes to prior authorization, how the request is handled can make or break the patient’s chances of getting an approval. That’s why many healthcare providers are shifting towards electronic approvals, because they are fast and accurate and have better chances of getting approved.
To understand it better, let’s look at the difference between electronic and manual prior authorization in detail.
Why are Healthcare Providers Switching to Electronic Prior Authorization?
By shifting to electronic systems, healthcare providers can save so much time, reduce the chances of errors, and create a better experience for patients. Electronic prior authorization has removed the hassle of back-and-forth work and made the process easier without unnecessary delays or rejections.
- Much Faster Approvals
Electronic systems can process prior authorization requests far quicker than phone calls and faxes ever could.
Approvals that used to take several days can now be handled within a few hours, which allows patients to start their treatment or get their prescriptions sooner.
- Reduced the Burden on Staff
Electronic prior authorization cuts down the mountain of paperwork that staff usually have to deal with.
By switching to an electronic process, they can spend less time chasing authorizations and more time on tasks, like helping patients and managing the overall flow of care.
- Staff Can Get Real-Time Updates
Providers no longer have to make repeated follow-up calls just to find out where a request stands.
Electronic systems allow them to get real-time updates, so staff can see the status of each prior authorization request and respond quickly if additional information is needed.
- No Delay in the Treatment of the Patients
When approvals happen faster, treatment plans stay on schedule. This is especially important for patients with chronic or serious conditions who can’t afford to wait days or weeks for a green light from their insurance company.
Conclusion
With the help of prior authorization services, healthcare providers can shift from a manual to a digital process, which is fast and efficient. By switching to digital systems, healthcare providers can reduce administrative work, improve patient experience, and make sure care is delivered on time.
Investing in an authorization management system has become a standard for modern healthcare operations.